
Source: Chinese Medical Journal
National In Vitro Diagnostic Network CAIVD
Endometrial cancer is the most common gynecological malignancy. Globally and in China, there are 417,400 and 71,100 new cases each year, respectively, and 97,000 and 17,100 deaths each year. Early identification of high-risk patients and precancerous lesions, achieving early cancer screening, and effectively detecting cancer progression and treatment are among the major issues in the current field of endometrial cancer diagnosis and treatment. For patients with postmenopausal bleeding and endometrial thickness exceeding 4 mm, only 8% of them have endometrial hyperplasia and endometrial cancer. The proportion of endometrial lesions in patients with recurrent postmenopausal bleeding only increased to 9%. The assessment of endometrial cancer mainly relies on invasive procedures, such as diagnostic curettage, hysteroscopy, and micro-detection of uterine cavity cytology and pathology, but the rate of missed diagnosis is relatively high. At present, there are no non-invasive screening programs recommended for clinical practice either at home or abroad.
Epigenetic silencing of tumor suppressor genes plays an important role in the occurrence and progression of cancer. There have been a large number of methylation studies on the occurrence and development of endometrial cancer. The latest research indicates that the self-collection of cervical exfoliated cells can improve the early diagnosis of endometrial cancer. Researchers have applied for multiple clinical trials of cervical cytology methylation detection for endometrial cancer and developed corresponding kits (NCT03744962, NCT04651738, NCT05290922 and NCT05290415). Based on these works, in this cohort study, the detection of CDO1 gene methylation (CDO1m) and CELF gene methylation (CELF4m) in cervical exfoliated cells was applied to screen postmenopausal women with suspected endometrial lesions. And explore the accuracy of cytological methylation with or without transvaginal ultrasound (TVS).
Objects and Methods
I. Research Object
This study is a cross-sectional study. Patients who visited the gynecology outpatient department of Peking Union Medical College Hospital from May 2020 to October 2021, were suspected of endometrial lesions, and were scheduled to undergo hysteroscopy were taken as the research subjects. Inclusion criteria: Age ≥40 years, based on the "Chinese Guidelines for Menopausal Management and Menopausal Hormone Therapy (2018)", and considered postmenopausal women according to clinical manifestations and examinations; According to the "Screening Standards for Endometrial Cancer", if endometrial lesions are suspected or as recommended by a clinician, hysteroscopy and biopsy should be performed. No previous treatment or surgical treatment for endometrial lesions has been received. Willing to undergo testing and sign the informed consent form; No invasive cervical cancer was found in the pre-hysteroscopic assessment. This study was approved by the Ethics Committee of Peking Union Medical College Hospital (Approval Number: ZS-2740), and all patients signed the relevant informed consent forms before undergoing the test.
The samples for cervical exfoliation cytology were obtained from the remaining 2 ml samples of patients who underwent traditional cytological examination and/or high-risk human papillomavirus (HPV) testing before surgery. The hysteroscopy of the patient was performed by a qualified surgeon from Peking Union Medical College Hospital under intravenous anesthesia. According to the patient's condition, biopsy, resection or diagnostic curettage was carried out on the endometrium and lesions. The cervical cytology and HPV tests of the patients as well as the histopathological assessment were completed and rechecked by the researchers.
Ii. Research Methods
The general conditions and clinical manifestations of patients related to the onset of endometrial cancer were collected by a dedicated case collection form. This study focuses on the following clinical indicators and examination results related to endometrial cancer, including age, menopausal status, number of pregnancies and deliveries, previous medical history, and body mass index. BMI, endometrial thickness evaluated by TVS within one month before hysteroscopy, and carbohydrate antigen 125 (CA125) value within one month before hysteroscopy. Combined with the medical history and clinical manifestations, determine whether there is a history of polycystic ovary syndrome (PCOS) based on domestic guidelines. In this study, a positive finding for TVS assessment was defined as an endometrial thickness of ≥5 mm (postmenopausal). Serum CA125≥35 U/ml is defined as abnormal. Abnormal uterine bleeding or postmenopausal vaginal bleeding is defined according to domestic guidelines.
Iii. Cytological Methylation Detection and Judgment
The experimental samples were all 2 ml of residual cervical cytology samples from the participants after cervical cancer screening. Sample collection should be carried out with the informed consent of the patient. After centrifugation of the cells, DNA was extracted from cervical exfoliated cells using the cell DNA extraction kit. The extracted nucleic acid was treated with the DNA bisulfite conversion kit. The converted DNA (Bis-DNA) was immediately subjected to PCR detection. Operate in accordance with the product manual of "Human CDO1 and CELF4 Gene Methylation Detection Kit (PCR-Fluorescence Probe Method)" (NCT05290922, Beijing Origin Juhuo Biotechnology Co., LTD.). PCR reactions were carried out using the SLAN-96S fully automatic medical PCR analysis system or the ABI 7500 real-time fluorescence quantitative PCR instrument. Reaction conditions: pre-denaturation at 96 ° C for 10 min; 45 cycles, denaturation at 94 ° C for 15 s, annealing at 64 ° C for 5 s, elongation and fluorescence acquisition at 60 ° C for 30 s; The instrument is cooled at 25 ℃ for 1 minute. After the reaction is completed, calculate ΔCt based on the Ct values of the CDO1 gene, CELF4 gene and the internal reference gene (ΔCt= CT-detected gene -Ct internal reference gene). The positive methylation judgment criterion is calculated using the Youde index scheme.
Iv. Statistical Analysis
Statistical analysis was conducted using the SPSS 26.0 statistical software package. Count data were expressed as cases (%), and the χ² test was used for comparison between groups. Measurement data that conform to the normal distribution are used
Result
I. Basic Information
A total of 143 patients were divided into the endometrial cancer group (56 cases) and the control group (87 cases), with ages of (59.27±6.45) and (61.07±8.26) years respectively (P=0.051). Among them, the control group included 80 cases of benign cancer, 3 cases of endometrial hyperplasia, and 4 cases of other cancers. The comparison of clinical features between the two groups is shown in Table 1.
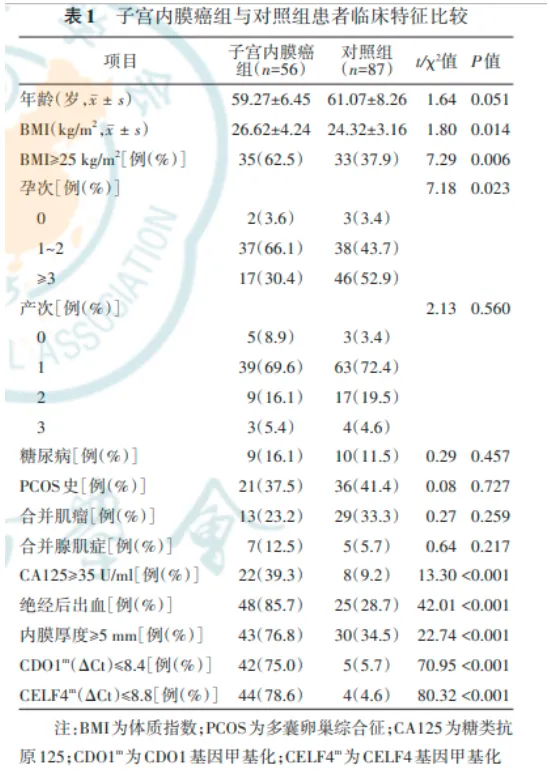
Ii. Analysis of Related Factors of Endometrial Cancer Incidence in Menopausal Women
Multivariate analysis revealed that CA125≥35 U/ml, menopausal bleeding, menopausal endometrial thickness ≥5 mm, CDO1mΔCt≤8.4, and CELF4mΔCt≤8.8 (based on Youde index) were related factors for the occurrence of endometrial cancer. The OR values (95%CI) were 33.23 (2.51-1,335.28), 8.41 (1.81-39.05), 14.45 (2.35-88.84), 17.34 (3.34-89.98), and 44.01 (6.79-285.25), respectively, and all P<0.05. Please refer to Table 2 for details.

Iii. Differences in endometrial thickness and the expression of CDO1m and CELF4m between the two groups of patients
The endometrial thickness of patients in the endometrial cancer group was 9.5 (5.0, 12.0) mm, which was higher than that of the control group (3.2 (2.0, 6.0) mm (Z=-5.10, P<0.001). The ΔCt value of the gene CDO1m level in the endometrial cancer group was 5.2 (2.5, 8.4), which was lower than 17.4 (14.6, 18.2) in the control group (Z=-7.97, P<0.001), while the ΔCt value of the gene CELF4m level in the endometrial cancer group was 4.9 (3.2, 8.5). It was lower than 16.4 (10.9, 17.9) of the control group (Z=-8.17, P<0.001).
Iv. Diagnostic efficacy in predicting endometrial cancer
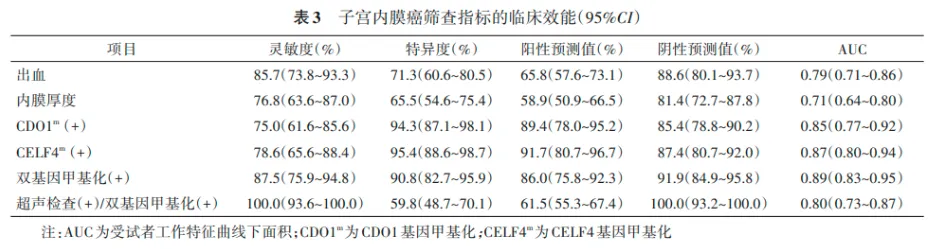
The ROC curves of various clinical indicators for screening endometrial cancer are shown in Figure 1. The AUC (95%CI) of endometrial thickness ≥5 mm, CDO1m (+), CELF4m (+), and double gene methylation (+) were 0.71 (0.64-0.80), 0.85 (0.77-0.92), 0.87 (0.80-0.94), and 0.89 (0.83-0.95), respectively. The AUC (95%CI) for ultrasound examination (+) or dual-gene methylation (+) was 0.80 (0.73-0.87).

V. Clinical Efficacy of Screening Indicators for Endometrial Cancer
The clinical efficacy of endometrial cancer screening indicators is shown in Table 3. The combined sensitivity of CDO1m and CELF4m dual genes was 87.5% (95%CI: 75.9% - 94.8%), the specificity was 90.8% (95%CI: 82.7% - 95.9%), and the positive predictive value was 86.0% (95%CI: The negative predictive value was 91.9% (95%CI: 84.9% - 95.8%), ranging from 75.8% to 92.3%. The sensitivity, specificity, positive predictive value and negative predictive value of diagnosing endometrial cancer by TVS endometrial thickness combined with dual-gene methylation were 100.0% (95%CI: 93.6% - 100.0%), 59.8% (95%CI: 48.7% - 70.1%), and 61.5% (95%CI:), respectively. 55.3% - 67.4%), 100.0% (95%CI: 93.2% - 100.0%).
Discussion
This study was the first to use a non-invasive liquid biopsy protocol for cervical exfoliated cytology gene methylation detection to screen for endometrial cancer in postmenopausal women, achieving higher accuracy than any other non-invasive detection protocol. Gene methylation combined with TVS examination further enhanced the sensitivity of endometrial cancer screening, confirming the value of this non-invasive screening protocol in clinical application. The study selected postmenopausal women with suspected endometrial lesions for enrollment. Firstly, the incidence of endometrial lesions was the highest in this population, thus enabling the comparison of the testing efficacy of various screening protocols with a smaller cohort size. Second, it can fully test the efficacy of clinical symptoms (postmenopausal bleeding) in the screening and diagnosis of endometrial cancer.
The selection of DNA methylation detection in cervical exfoliated cells for the screening and diagnosis of endometrial cancer is an important innovation in this study. Previous studies have carried out exfoliated cells for cytopathological analysis, detection of endometrial cancer target genes, diagnosis of genetic syndromes, exosome analysis, MSI detection, and multi-omics detection. However, no relevant research on epigenetic analysis of exfoliated cells has been carried out yet, let alone reliable screening protocols applied in clinical practice. On the other hand, the work of detecting endometrial cancer using blood ctDNA lacks sufficient sensitivity due to the insufficient abundance of tumor cells. It is only suitable for a few cases of endometrial cancer, such as high-grade endometrial cancer (type II endometrial cancer accounting for less than 10% of endometrial cancer) and advanced endometrial cancer, and is not suitable for early screening and diagnosis of endometrial cancer. Cervical exfoliated cells have many outstanding advantages in the screening and diagnosis of endometrial cancer: (1) Completely non-invasive. Except for women who have no sexual life, sampling will not cause any damage to the vagina or cervix. It is even simpler and safer than collecting peripheral blood. (2) It is convenient to obtain materials. The accuracy is no less than the results of samples taken by doctors or testers. (3) The cell quantity is sufficient. A small amount of vaginal irrigation fluid is fully capable of performing methylation detection and is highly consistent with histological results.
Cervical exfoliated cytology for endometrial cancer screening requires the selection of reliable target genes to distinguish the tumor specificity of positive results, that is, whether the screening results indicate cervical cancer or endometrial cancer. If it is endometrial cancer, can different types of endometrial cancer be considered for inclusion? Studies have shown that choosing the appropriate target genes can achieve differentiation. Previous studies have used cervical exfoliated cytology to distinguish endometrial cells from cervical cells and have carried out work on exosomes and metabolomics of endometrial cells. The accuracy of cervical exfoliated cells in evaluating endometrial lesions is no less than that of uterine cavity cytology (or irrigation fluid) obtained through invasive procedures. The relationship between the epigenetic alterations of the target genes CDO1 and CELF4 selected in this study and endometrial cancer has been supported by the literature.
TVS has become the preferred screening method for the clinical diagnosis of endometrial diseases in postmenopausal women due to its advantages of being non-invasive, economical and easy to operate. TVS has a high sensitivity for screening endometrial cancer, but its specificity is low, often resulting in unnecessary invasive operations. In this study, cytological methylation detection combined with TVS can further improve the sensitivity of endometrial cancer screening. However, due to the low specificity of TVS, the combined detection of the two failed to achieve a higher level of specificity. If TVS is combined, some specificity will be sacrificed and the possibility of invasive operation will increase. Whether this situation can be repeated and improved still needs to be confirmed by large-scale cohort studies.
The most innovative value of this study lies in the application of cytological methylation detection for the screening of endometrial cancer. This study also has some drawbacks, including the small overall sample size and the urgent need for generalization in large cohorts. This will be further met and supplemented in the large-scale multi-center prospective study (NCT05290415) conducted by the researchers.
In conclusion, the research provides a simple, non-invasive and highly sensitive screening method for endometrial cancer in postmenopausal women through DNA methylation in cervical exfoliated cytology, which urgently needs to be further verified in large-scale clinical studies.
Cite this article
Kong Linghua, Xiao Xiaoping, Wan Ru, et al. Application Value of DNA methylation detection in endometrial Cancer Screening in Postmenopausal women [J]. Chinese Medical Journal, 2023, 103(12) : 907-912. DOI: 10.3760/cma.j.cn112137-20220929-02058.
0756-8699969
Address: No. 88, Shuian 1st Road, Nanping Science and Technology Park, Xiangzhou District, Zhuhai City, Guangdong Province
Email: marketing@biori.com
Wechat official account |
Product consultation |
Join us |
Video Account |






